Immune cells for suppressing the deterioration of multiple sclerosis identified
Plasmablastas suppress deterioration in multiple sclerosis (MS)
A group of researchers at Immunology Frontier Research Center, Osaka University clarified that inhibitory cytokine, interleukin-10 (IL-10) secreted from B cell group, referred to as plasmablastas, suppress deterioration in multiple sclerosis (MS).
- MATSUMOTO Masanori , Assistant Professor
BABA Yoshihiro , Associate Professor
KUROSAKI Tomohiro , Professor
The immune system in the body differentiates between "self" and "non-self" and only gets rid of things that are "non-self". However, once this immune system has broken down, the system attacks the self's normal cells and tissues, causing autoimmune disorders such as multiple sclerosis (MS), rheumatoid arthritis (RA), and systematic erythematodes. MS is one of central nervous system demyelinating disorders which causes inflammation in the brain, spinal marrow, and optic nerves, leading to neurological deterioration such as motor weakness and sensory impairment. In Japan, MS is estimated to occur in out of 8 ~ 9 persons per 100,000 and is designated as an intractable disease. Although the mechanism for development and deterioration of MS has not been clarified, MS is thought to be caused by the destruction of the myelin sheath by immune cells. In recent years, it has been reported that B cells producing IL-10, referred to as regulatory B cells, suppress experimental autoimmune encephalomyelitis (EAE) in MS mouse models. However, it has not been clarified under which B cell group regulatory B cells are classified and it has been unknown through what mechanism they suppress encephalomyelitis. This group's research clarified that IL-10-producing plasmablasts derived from B cells inhibited function of dendritic cells, thereby suppressing the deterioration of encephalomyelitis. From these findings, if the differentiation of IL-10-producing plasmablasts can be controlled, this will lead to the development of new methods of treatment for MS.
Abstract
B cells can suppress autoimmunity by secreting interleukin-10 (IL-10). Although subpopulations of splenic B lineage cells are reported to express IL-10 in vitro, the identity of IL-10-producing B cells with regulatory function in vivo remains unknown. By using IL-10 reporter mice, we found that plasmablasts in the draining lymph nodes (dLNs), but not splenic B lineage cells, predominantly expressed IL-10 during experimental autoimmune encephalomyelitis (EAE). These plasmablasts were generated only during EAE inflammation. Mice lacking plasmablasts by genetic ablation of the transcription factors Blimp1 or IRF4 in B lineage cells developed an exacerbated EAE. Furthermore, IRF4 positively regulated IL-10 production that can inhibit dendritic cell functions to generate pathogenic T cells. Our data demonstrate that plasmablasts in the dLNs serve as IL-10 producers to limit autoimmune inflammation and emphasize the importance of plasmablasts as IL-10-producing regulatory B cells.
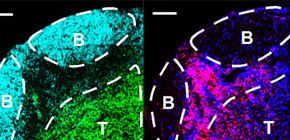
Figure 1. CD138 + CD44 hi cells are dominant IL-10-producing B lineage cells during EAE
Figure 2. CD138 + cells in the draining lymph nodes are plasmablasts
Figure 3. Deficiency of plasmablasts in mice leads to exacerbated EAE
Figure 4. Plasmablasts are colocalized with dendritic cells in the extrafollicular region
Figure 5. Plasmablast-derived IL-10 inhibits dendritic cell functions
Figure 6. Plasmablast-derived IL-10 inhibits the generation of pathogenic T cells
To learn more about this research, please view the full research report entitled " Interleukin-10-producing plasmablasts exert regulatory function in autoimmune inflammation " at this page of the Immunity website.
Related Link
