Predicting heart failure with longitudinal urine patterns and its changing
Researchers from Osaka University find that stable, long-term elevation in urinary albumin excretion in healthy Europeans is associated with a high risk of new-onset heart failure and mortality.
They say that an ounce of prevention is worth a pound of cure; knowing which preventive treatment to administer to which patient could undoubtedly up that yield. Now, an international research team led by Osaka University has identified an important treatment target that could help prevent patients from developing a serious heart condition in the future.
In a study published last month in the European Journal of Heart Failure, the research team reported the identification of long-term patterns in levels of kidney health indicators in healthy European adults, and the impact of these patterns on the risk of new-onset heart failure.
One in five people will develop HF in their lifetime, and impaired kidneys are one of the most critical risk factors for developing this condition. Because of this connection, it is common practice to monitor markers of kidney health in patients who are at risk of developing heart failure.
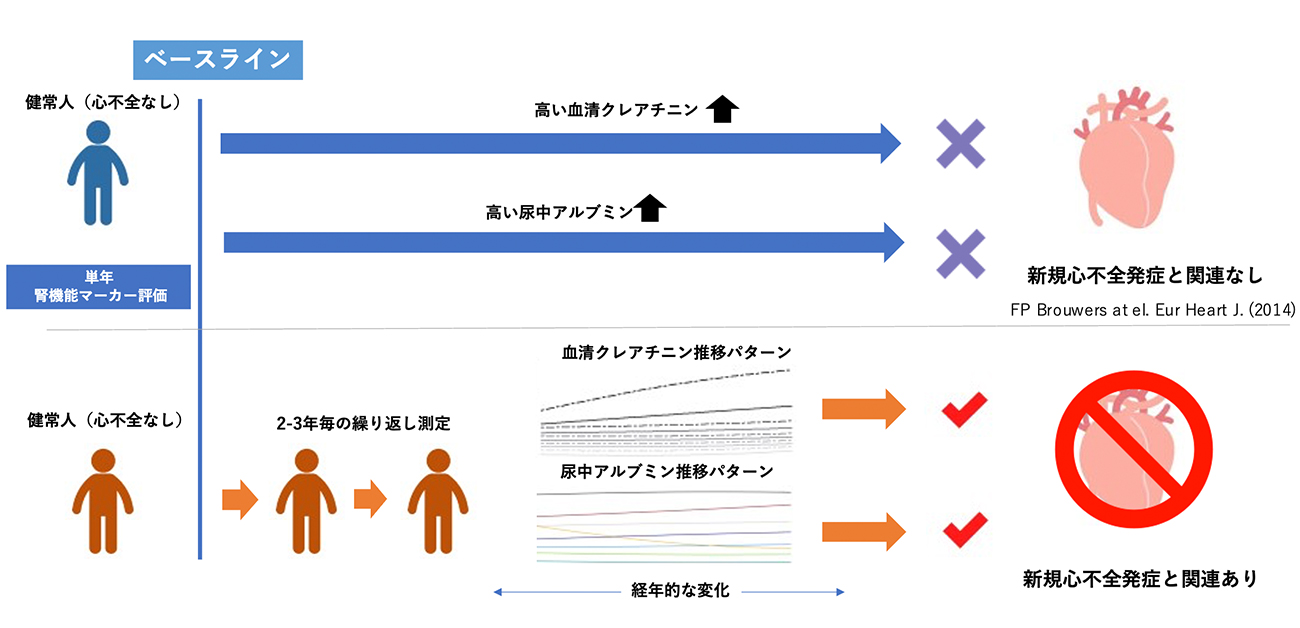
“Day-to-day or short-term fluctuations in renal biomarkers are well-known,” says lead author of the study Dr.Ryoto Sakaniwa. “However, the connection between long-term patterns in biomarker levels and the risk of heart failure is unknown.”
To address this, the researchers looked at levels of two common markers of kidney health––urinary albumin excretion (UAE) and serum creatinine––in almost 7000 patients from the Dutch study Prevention of Renal and Vascular End-stage Diseases (PREVEND). Patterns in UAE and serum creatinine levels were tracked over 11 years and investigated for their association with new-onset heart failure and death.
“The results were very clear,” explains Dr. Jasper Tromp, senior author. “While most participants had stable low UAE or serum creatinine, those with persistently high UAE had a statistically higher risk of new-onset heart failure or all-cause mortality. Interestingly, annual levels of renal biomarkers were remarkably stable year to year across the 11 years of follow up”
Stable serum creatinine levels over time were associated with heart failure, but not with a higher risk of death. More detailed analysis showed that patients with persistently higher UAE or serum creatinine levels were more likely to be older and male, and to have conditions such as diabetes, previous heart attack, or dyslipidemia.
“Our results highlight the importance of the heart-kidney link in heart failure by showing that patients with persistently worse renal function, as indicated by higher UAE or serum creatinine levels, are at a higher risk of heart failure or mortality,” says Sakaniwa. “Reducing these renal biomarkers could help prevent heart failure.”
The findings from this study suggest that reducing UAE could help lower the risk of future heart failure and death in these patients. Given that one in five men and women will develop heart failure during their lifetime, these findings could have an important impact on preventive medicine and should be confirmed in non-European populations.
Fig. 1
Graphic abstract for current study
Credit: R.Sakaniwa at el., European Journal of heart failure 2023
Fig. 2
Trajectories of serum creatinine subtype and its incident rate of new heart failure onset
Credit: R.Sakaniwa at el.,
Fig. 3
Trajectories of urinary albumin excretion subtype and its incident rate of new heart failure onset. - Lowering Urinary albumin excretion (class 5) reduces the risk of new heart failure onset (vs. class 6) -
Credit: R.Sakaniwa at el.,
The article, “Trajectories of renal biomarkers and new onset heart failure in the general population: Findings from the PREVEND study,” was published in European Journal of Heart Failure at DOI: https://doi.org/10.1002/ejhf.2925.
