A donation that could help cure blood cancer
Researchers from Osaka University compare two cell transplantation strategies for eradicating cancer in a subset of acute myeloid leukemia patients
Acute myeloid leukemia (AML) is a common type of blood cancer that has a relatively low survival rate. It is particularly deadly for patients suffering from refractory and relapsed AML (R/R AML), meaning their cancer has stopped responding to treatment and has returned after a period of remission. In a recently published article in Leukemia, a group led by researchers at Osaka University compared the survival rates of R/R AML patients treated with two different forms of donor transplantation therapy to determine if one was more effective in this population.
R/R AML is in particular need of efficient and powerful therapeutic strategies, because fewer than 10% of patients currently live for 5 years or longer. A treatment called hematopoietic stem cell transplantation (HSCT) is the only existing option. This method is allogeneic, meaning the stem cells are obtained from someone other than the patient. HSCT can be very effective and essentially cure the cancer, but the conditions need to be ideal. Of crucial importance is that the disease is in complete remission, because patients in non-remission often relapse following treatment. Donor selection is important, and transplantation from a human leukocyte antigen matched related (MRDT) donor has been considered to be a standard donor.
Another transplantation method similar to MRDT is known as cord blood transplantation (CBT) with comparable effects. However, previous studies have suggested that CBT may be more effective for R/R AML patients with non-ideal conditions.
“We believe CBT would be a great treatment option for R/R AML patients in non-remission given the circumstances,” says lead author of the study Yoshimitsu Shimomura. “However, there are currently limited data for how this subset of patients would respond to CBT.”
To establish such a dataset, the team examined survival data of 1,738 adult non-remission R/R AML patients who were given CBT and compared them with those of 713 similar patients who were given MRDT. These comparisons were made by examining the 5-year progression-free survival (PFS) rates of these Japanese patients.
“Before comparing PFS rates, we performed propensity score matching,” explains Shimomura. “This took into account factors such as patient age, sex, years of treatment, and others to ensure all comparisons were as fair as possible and no biases were introduced.”
Interestingly, the MRDT-treated patients had an 18.1% 5-year PFS, while this value for the CBT-treated patients was 25.2%. The difference was statistically significant, meaning there were enough data in the study to have confidence that the results are representative and meaningful.
“CBT compared with MDRT had a more pronounced decrease in relapse rate than increase in NRM,” describes Shimomura.
These intriguing data support CBT as a potential superior alternative to MRDT for patient prognosis and thus provide evidence which may influence clinical guidelines on R/R AML treatment. Future studies will investigate if genetic factors play any roles in patients’ responses to these two transplantation methods. Additionally, patient quality of life will be considered to optimize therapeutic development for this deadly disease.
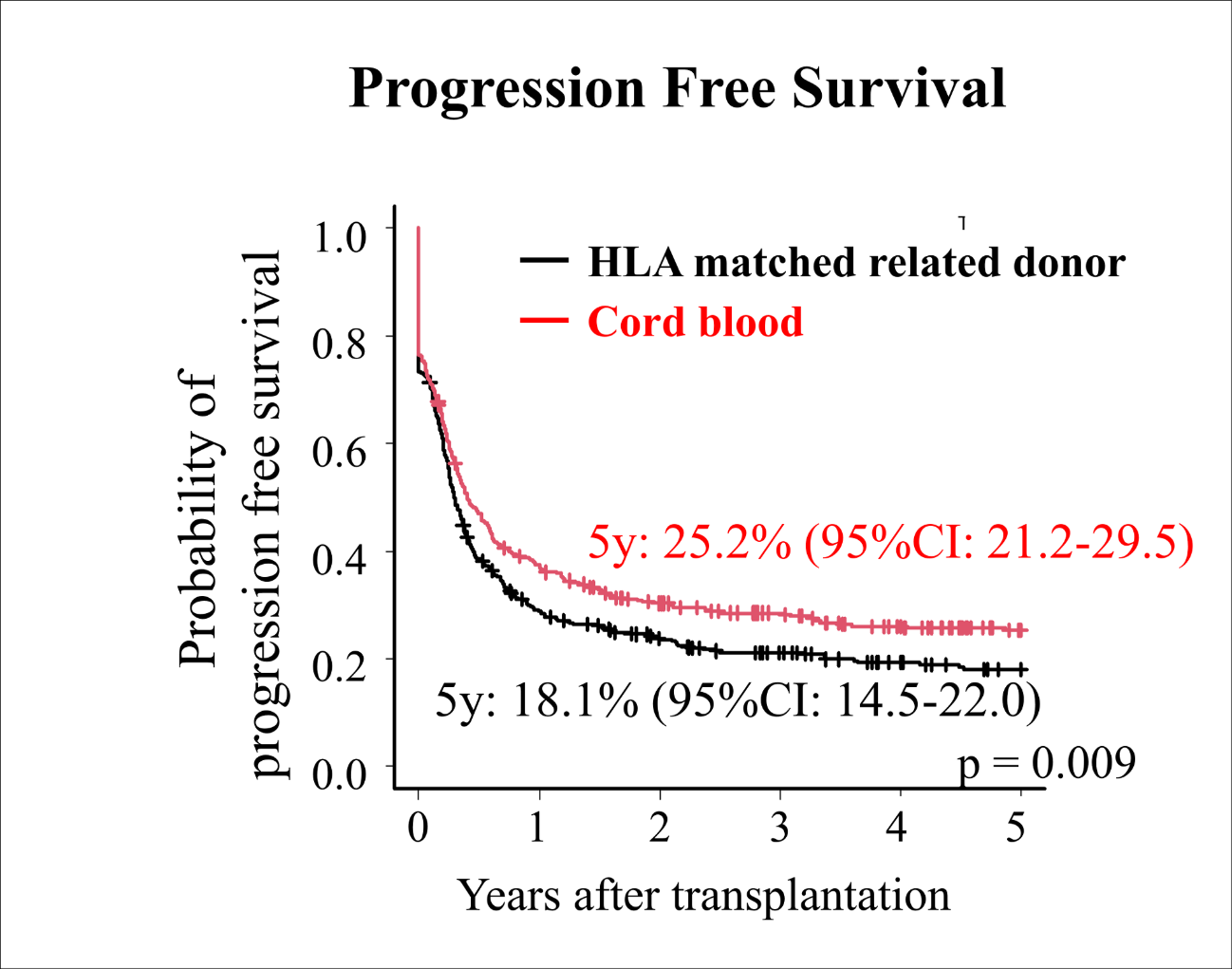
Fig.1 Progression free survival comparing cord blood transplantation and HLA matched related donor transplantation
The article, “Comparing cord blood transplantation and matched related donor transplantation in non-remission acute myeloid leukemia,” was published in Leukemia at DOI: https://doi.org/10.1038/s41375-021-01474-0.
