Elucidating the pathological mechanisms of Helicobacter pylori-induced gastritis
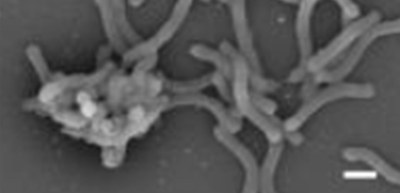
A group of researchers from the Research Institute for Microbial Diseases of Osaka University has revealed how Helicobacter pylori (H. pylori) develops gastritis, namely that H. pylori extracts cholesterol from the host, converts it to unique cholesteryl glucosides, and exacerbates gastritis through the interaction with C-type lectin receptors.
H. pylori is a gastrointestinal pathogen that infects about half of the world’s population at some time in their life. Since infection with H. pylori increases the risk of gastritis and stomach cancer, antibiotic eradication of H. pylori is an established therapy. Recently, however, such methods are limited due to the emergence of drug resistance and microbial dysbiosis (or the imbalance of microbial species due to a reduction in microbial diversity within certain bodily microbiomes). Thus, viable alternative eradication strategies, such as concomitant or alternative therapy regimens, were anticipated. In addition, how H. pylori develops gastritis was unknown.
H. pylori-induced gastritis requires activation of T cells, a major part of the immune system that is activated by dendritic cells (DCs). However, H. pylori avoids detection by the pattern recognition receptors, Toll-like receptors (TLRs), by modifying ligands of TLRs. Recognition of molecular signatures of potential pathogens via TLRs activates DCs, leading to the initiation of adaptive immunity; however, the mechanism how H. pylori causes T-cell activation was not fully understood.
This group isolated lipid extracts from H. pylori and found that the isolated lipid extracts were Helicobacter pylori glycolipids, cholesteryl acyl α-glucoside (αCAG), and cholesteryl phosphatidyl α-glucoside (αCPG), and that αCAG recognized by macrophage-inducible C-type lectin receptor (Mincle, gene symbol: Clec4e) activated immune response.
During chronic infection, H. pylori–specific T cells responded and the severity of gastritis was improved in Mincle-deficient mice, and antibody (Ab) blockade of Mincle resulted in the suppression of T cell responses and gastritis. Chronic gastritis was observed in wild-type mice after infection of H. pylori; however, the severity of gastritis was ameliorated in Clec4e gene knockout mice. The researchers also found that αCPG was identified by ligands for DC immunoactivating receptor (DCAR; gene symbol Clec4b1) and potently activated human DCs.
A mutant H. pylori strain lacking Hp0421 exhibited an impaired ability to cause gastritis, showing that the production of cholesteryl glucosides (αCAG and αCPG) by H. pylori is required for its virulence to promote gastritis.
HP0421, a cholesterol α-glucosyltransferase gene, belongs to the glycosyltransferase family 4 and is present only in pylori and some Helicobacter species. The Hp0421 gene encodes cholesteryl-α-glucoside transferase (CGT) and plays an important role in the synthesis of αCAG and αCPG. H. pylori extracts cholesterol from a host and adds glucose to it using its glucosyltransferase. This group elucidated molecular mechanisms by which H. pylori takes in cholesterol in the host and turns it into inflammation chemical compounds, such as αCAG and αCPG, causing gastritis.
Antibody (Ab) blockade of Mincle in the host defense immune system and the development of vitamin D derivatives that inhibit enzyme Hp0421, which is assimilated by H. pylori, will provide a harmless regimen for the prevention of H. pylori–induced gastritis and subsequent malignancy.
α-cholesterylglucoside (αCAG)
Figure 1
Figure 2
Figure 3
Figure 4
The article, “Helicobacter pylori metabolites exacerbate gastritis through C-type lectin receptors,” was published in Journal of Experimental Medicine at DOI: https://doi.org/10.1084/jem.20200815.
Related links
Yamazaki Laboratory, Department of Molecular Immunology, RIMD, Osaka University (link in Japanese)
