Sleep duration and quality in patients with chronic kidney disease influence progression to dialysis
Large-scale epidemiologic studies of 1,601 patients with CKD over median 4 year follow-up
A group of Osaka University researchers led by Lecturer Ryohei Yamamoto at the Health and Counseling Center and Professor Yoshitaka Isaka at the Graduate School of Medicine clarified, using results of surveys from 1,601 CKD patients with kidney dysfunction, that CKD patients who had poor sleep quality and CKD patients with shorter (5 hours or less) or longer (more than 8 hours) sleep duration were highly likely to progress to end stage renal disease and require dialysis.
It has been reported that sleep disorders such as shorter sleep duration are risk factors for developing CKD in subjects with normal kidney function. Sleep disorders are a risk factor of developing various lifestyle-related diseases, but the importance of good quality sleep in the prevention of CKD has not been assessed until recently. Although CDK characterized by persistent proteinuria and reduced kidney function is highly likely to progress to dialysis, studies were performed for some 400 patients in the U.S.
Using data from mandatory annual health examinations of employees at Osaka University, the group reported that short sleep duration of 5 hours or fewer is a risk factor of proteinuria in 2011. ( https://doi.org/10.1053/j.ajkd.2011.08.032 ) Later, similar results have been reported in the country and overseas and was clarified that short sleep duration was a risk of developing CKD in subjects with normal kidney function.
The Chronic Kidney Disease Japan Cohort (CKD-JAC) Studies conducts a large-scale epidemiologic studies to follow up some 3,000 outpatients with CKD in 17 hospitals in Japan. The group at Osaka University studied 1,601 patients who participated in the Chronic Kidney Disease Japan Cohort (CKD-JAC) and answered self-report questionnaires, the Japanese version of the Pittsburgh Sleep Quality Index (PSQI-J), to assess how many CKD patients progressed to dialysis after a mean follow-up of about 4 years. As a result, they clarified that good quality sleep was important for CKD patients just like it is for healthy individuals.
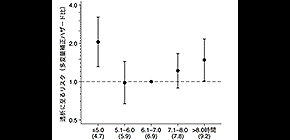
CKD patients who had poor sleep quality had some 30 percent higher risk of progressing to dialysis than CKD patients who had normal sleep quality. In addition, patients with a shorter (5 or fewer hours) or longer (more than 8 hours) sleep duration were associated with 1.5-2.1 times the risk of progressing to dialysis compared with patients with a sleep duration of about 7 hours.
This study clarified that patients who had poor sleep quality and patients with shorter or longer sleep duration had a higher risk of progressing to dialysis. It is anticipated that the risk of progression to dialysis in patients with sleep problems can be reduced by receiving treatment according to the cause.
The number of CKD patients who progress to dialysis, which is expensive treatment, has been on the rise in recent years. In establishing therapeutic strategies for suppressing the rise in treatment costs, good sleep duration is surely a notable lifestyle factor.
Abstract
Background and objectives Shorter or longer sleep duration and poor sleep quality are risk factors for numerous cardio-metabolic diseases, cardiovascular disease, and mortality in subjects with normal kidney function. The association of sleep duration and sleep quality with health outcomes in patients with CKD remains uncertain.
Design, setting, participants, & measurements A 4-year prospective cohort study in 17 nephrology centers in Japan, the CKD Japan Cohort (CKD-JAC) Study, assessed an association of self-reported sleep duration and sleep quality, on the basis of the Pittsburgh Sleep Quality Index (PSQI) questionnaire, with incidence of ESKD in 1601 patients with eGFR 10–59 ml/min per 1.73 m 2 using multivariable-adjusted Cox proportional hazards models.
Results Baseline sleep duration and PSQI global score for the 1601 patients were mean±SD 7.0±1.3 hours and median 4 (interquartile range, 3–7), respectively. Poor sleep quality (PSQI global score ≥6) was common (n=588 [37%]). During a median of 4.0 (2.6–4.3) years of the follow-up period, 282 (18%) patients progressed to ESKD. After adjusting for age, sex, eGFR, urinary albumin excretion, smoking status, body mass index, history of diabetes and cardiovascular disease, systolic BP, blockade of the renin-angiotensin system, use of hypnotics, and Beck depression inventory score, both shorter (≤5 hour) and longer (>8 hour) sleep duration were associated with ESKD (adjusted hazard ratios [95% confidence intervals] for ≤5.0, 5.1–6.0, 6.1–7.0, 7.1–8.0, and ≥8.0 hours were 2.05 [1.31 to3.21], 0.98 [0.67 to 1.44], 1.00 [reference], 1.22 [0.89 to 1.66], and 1.48 [1.01 to 2.16]), suggesting a U-shaped relationship between sleep duration and ESKD. PSQI global score ≥6 was also associated with incidence of ESKD (adjusted hazard ratios [95% confidence intervals] for PSQI global score ≤5 and ≥6 were 1.00 [reference] and 1.33 [1.03 to 1.71]).
Conclusions Shorter (≤5 hour) and longer (>8 hour) sleep duration and poor sleep quality (PSQI global score ≥6) were associated with ESKD in patients with CKD
Figure 1 . An association between self-reported sleep duration and incidence of end-stage kidney disease requiring kidney replacement therapy in 1,601 patients with CKD, who were enrolled in the CKD-JAC study, a 4-year prospective cohort study, The patients with short (≤5 hours) and long (>8 hours) sleep duration at thier baseline visit were at significantly higher risk of ESKD, compared with those with sleep duration of 6.1-7.0 hours.
The article "Sleep Quality and Sleep Duration with CKD are Associated with Progression to End Stage KidneyDisease” was published in the Clinical Journal of American Society of Nephrology at DOI: https://doi.org/10.2215/CJN.01340118 .
Related links
- Kidney Internal Medicine, Graduate School of Medicine, Osaka University (link in Japanese)
