
Researchers find adult endothelial stem cells that can make fully functional blood vessels
Research team centered at Osaka University uses newly identified blood vessel stem cells to repair injured blood vessels and treat vascular disorders
The proper function of blood vessels is essential to life: blood vessels are responsible for transporting oxygen-rich red blood cells, nutrients, and immune cells throughout the body, to name just a few functions. Defects in blood vessels can correspondingly lead to a variety of life-threatening diseases. Stem cells, which are undifferentiated cells that can generate new tissues, have significant potential in regenerative medicine and treating various disorders. In blood vessels, the existence of tissue-resident stem cells has been intensely debated. A research team centered at Osaka University may now have discovered the elusive stem cell, providing evidence for adult vascular endothelial stem cells (VESCs) capable of generating fully functional blood vessels.
The research team had previously identified a population of endothelial cells (ECs), isolated from the inner most layer of blood vessels, with properties resembling those of stem cells. The cells were actually isolated by functional analysis, so the team was interested in finding molecular markers that specifically define endothelial stem cells. The research was reported in Cell Stem Cell .
“Our approach was to look for a cell-surface protein that is highly expressed in the endothelial stem-like population, but not in other ECs,” explains Nobuyuki Takakura, who led this study. “Once we found a clear stem marker of ECs, we could then sort the cells based on the proteins expressed on their surface. This would theoretically allow us to isolate a homogeneous pool of candidate endothelial stem cells.”
The researchers found a highly abundant glycoprotein, called CD157, expressed in the small fraction of EC population. After isolating just the ECs that expressed CD157, they set out to determine whether they were truly VESCs. The key characteristic of stem cells is their ability to regenerate themselves, so they hypothesized that the CD157-positive ECs would be able to form new blood vessels. The team tested this idea by experimentally injuring mice, damaging the blood vessels that supply blood to the liver, and injecting them with CD157-positive ECs isolated from the liver.
“The results were more than we could have hoped for,” Takakura adds. “A month after transplantation, the CD157-enriched cells generated fully functional portal veins, portal venules, sinusoids, hepatic venules, and arteries—essentially, every type of blood vessel found in a healthy liver. We were very encouraged by the result, so we followed up by injecting mice with just one cell each. The success rate was smaller, but even a single cell was enough to reconstitute their blood vessels.”
In addition to repairing injured tissue, stem cells are crucial to maintaining healthy tissue. As further confirmation that they had discovered a VESC, the team used a fluorescent reporter to follow the fate of these cells in non-injured healthy mice. A year later, the cells continued to replenish normal blood vessel tissue in the liver—precisely what would be expected of functioning, native stem cells.
Following the successful liver repair experiments, the team sought to determine how versatile the cells might be in treating other blood vessel-related diseases. Hemophilia A, a rare bleeding disorder in which blood is unable to clot properly, is caused by a genetic mutation that prevents liver blood vessels from making clotting factor VIII (FVIII). When VESCs collected from healthy mice were injected into mice with hemophilia A, the cells began generating new liver blood vessels—and the level of FVIII in the blood shot up, from less than 1% of normal to over 60%.
Notably, the therapeutic potential of these cells does not appear to be limited to liver defects. The researchers also used VESCs from muscle tissue to treat limb ischemia in mice, where a lack of oxygenated blood can lead to tissue damage and foot necrosis. The study potentially represents a turning point in cell-based therapies for blood vessel disorders.
“Our findings show that CD157-positive vascular endothelial stem cells give rise to a hierarchy of cell types that can repair vascular injury and maintain the normal blood vessel architecture,” Takakura says. “We believe these findings represent an entirely new way of thinking about how blood vessels are formed and, ultimately, how stem cells can be used to treat disorders related to blood vessel malfunction.”

Fig. 1: Vascular Endothelial stem cell (VESC) system in the liver. Vascular injury induces activation of VESCs. VESCs proliferate and replace the damaged ECs. New blood vessels are derived from VESCs. (credit: 2018 Wakabayashi et al., Cell Stem Cell 22, 1-14 .)
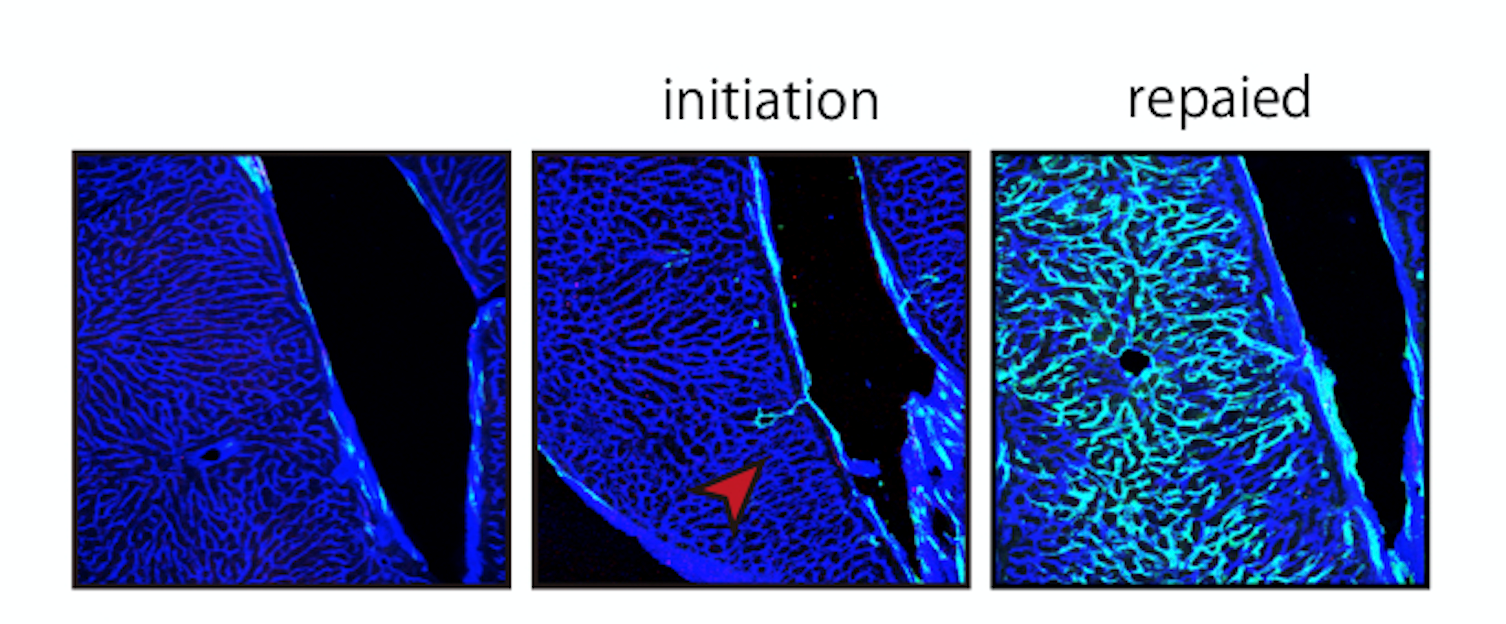
Fig. 2: Linage tracing of VESC. New blood vessels emerged from VESC (shown in green). Most of the endothelial cells (ECs) are replaced by ECs derived from VESC. (credit: 2018 Wakabayashi et al., Cell Stem Cell 22, 1-14 .)
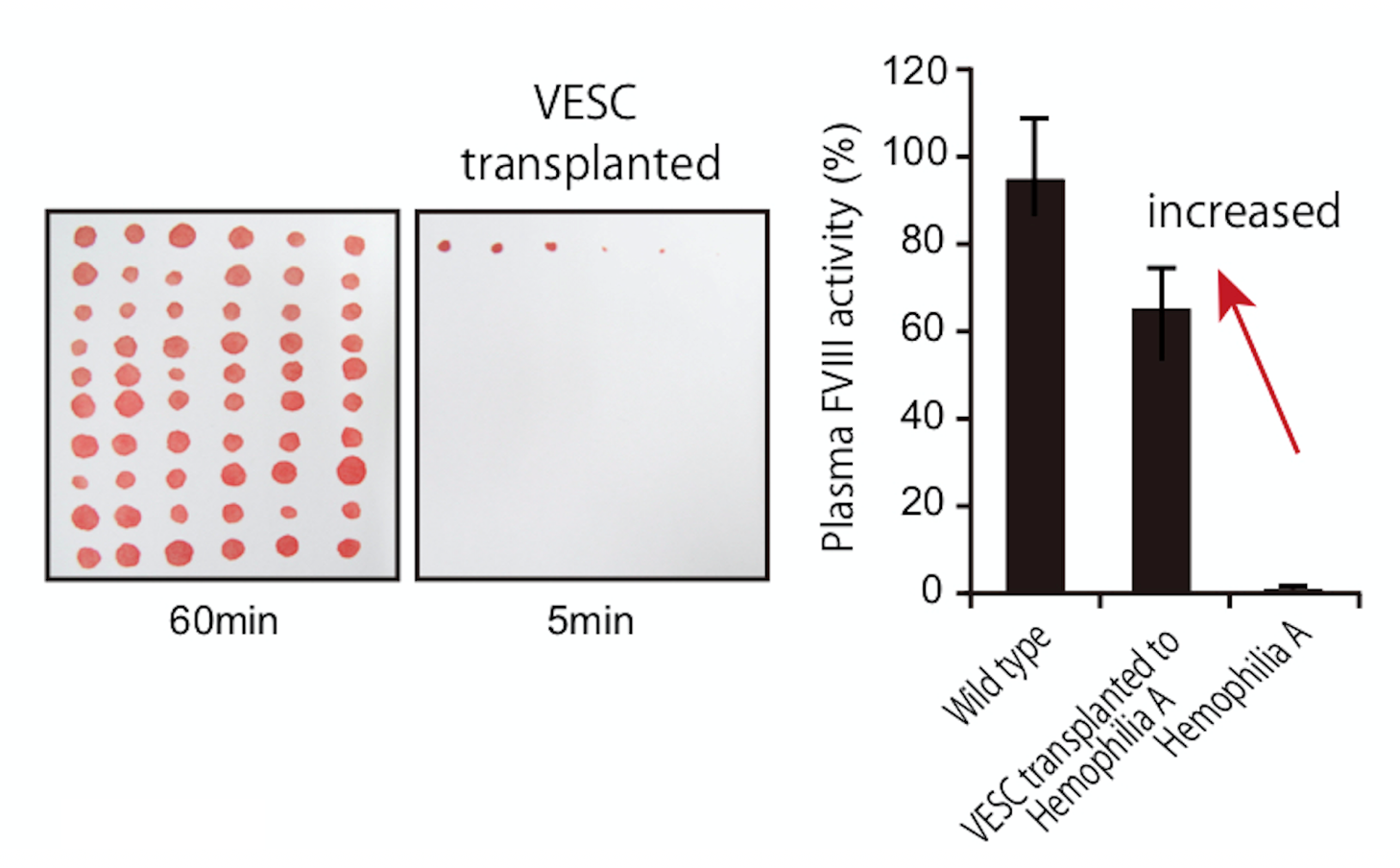
Fig. 3: Bleeding stopped very quickly in mice which underwent VESC transplantation. Plasma FVIII activity in hemophilia A mice after transplantation of VESCs increased to therapeutic level. (credit: 2018 Wakabayashi et al., Cell Stem Cell 22, 1-14 .)
To learn more about this research, please view the full research report entitled " CD157 Marks Tissue-Resident Endothelial Stem Cells with Homeostatic and Regenerative Properties " at this page of Cell Stem Cell .
Related links
