Drugs that regenerate lost periodontal tissue
Medical care for enjoying a life that one considers normal
Professor Shinya Murakami, Graduate School of Dentistry, Osaka University
“The disease with the largest number of patients worldwide is periodontal disease. If we look across the planet, there are only a few humans not affected by this disease.” This is what the Guinness Book of Records states. In Japan, 80% of adults are considered to have periodontal disease, including mild cases, and it is the most frequent cause of loss of teeth in middle-aged and older people. Although it is not immediately life-threatening, it may seriously affect the quality of life (QOL). Periodontal disease may be termed a national disease or even a humanity disease, and we consider it difficult to completely cure once contracted and that lost tissues cannot be restored. However, Professor Shinya Murakami of Osaka University Graduate School of Dentistry developed the first agent to induce periodontal tissue regeneration and confirmed it to be effective. In September 2016, the agent was approved by the Ministry of Health, Labour and Welfare and began to be covered by health insurance. Approximately 76,000 kits of the agent have been shipped under the name Regroth and used for patients with periodontal disease.

Turning back the clock of damaged cells and tissues
What does “periodontal tissue” that is destroyed by periodontal disease refer to?
“Periodontal tissue” is the tissue that supports teeth in the mouth, and consists of the gingiva (gum), periodontal ligament, cementum, and alveolar bone. The surface of the roots of teeth is covered by hard cementum, which is wrapped by the thin and tender periodontal ligament. The periodontal ligament is guarded by the hard alveolar bone, which is further surrounded by the gingiva.
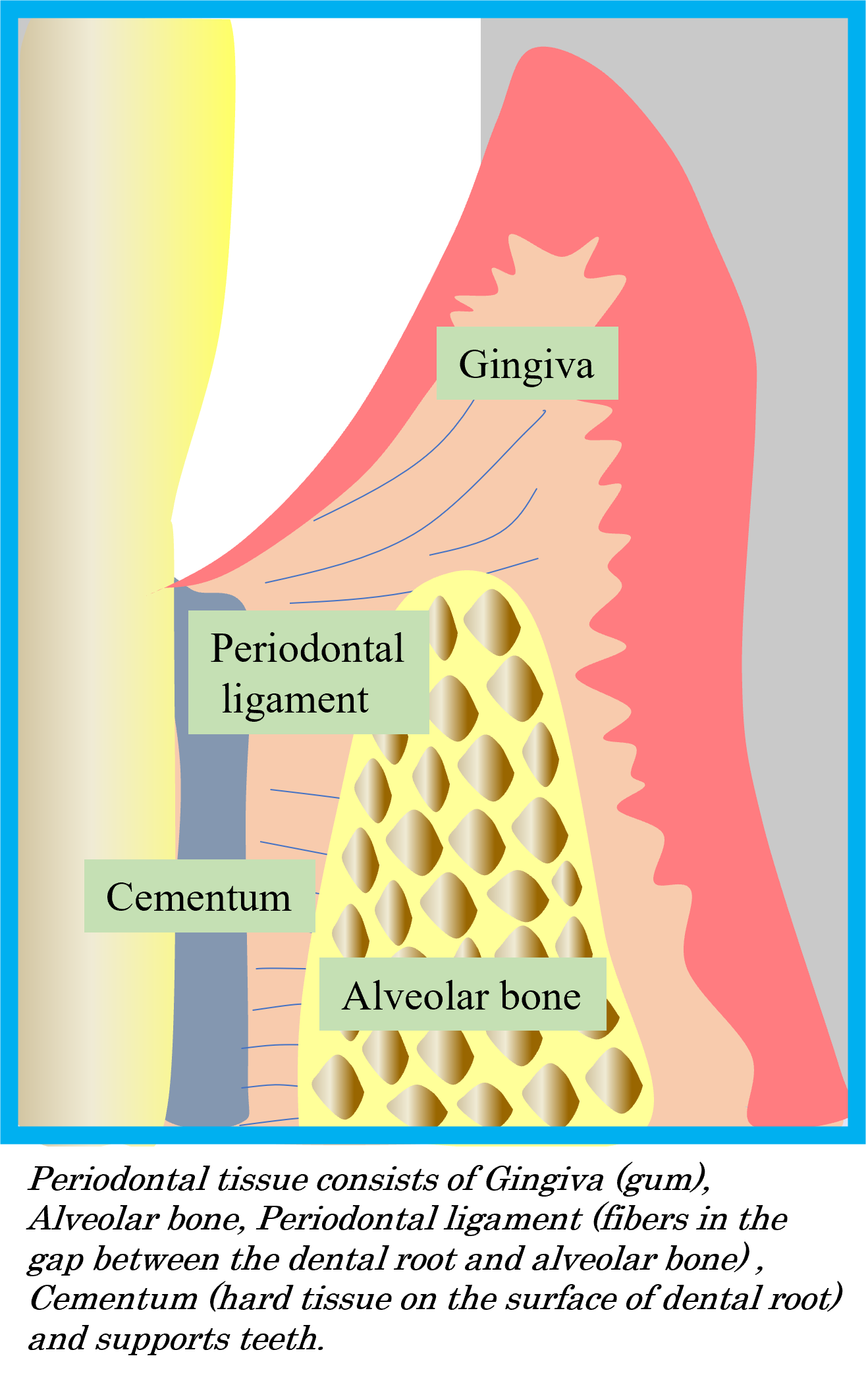
The periodontal ligament is only 0.1-0.2 mm thick, but is made of flexible collagen fibers, both ends of which enter the cementum and alveolar bone to firmly fix the teeth. There are also nerves that sense pressure in the periodontal ligament, and they send information about resistance of the material being chewed, i.e., whether it is soft or hard, to the brain.
However, if the mouth is unclean, several hundreds of millions of bacteria of hundreds of species grow between the teeth and gum, and dental plaque, which is aggregates of bacteria, cause gingivitis or inflammation of the gum. If it advances, the space between the tooth and gum, called the pocket, deepens progressively, enabling bacterial to further proliferate, setting off a vicious cycle. If the alveolar bone is lysed, the condition is termed periodontitis, and in the terminal stage, the alveolar bone is destroyed to the end of the dental root, making extraction of teeth inevitable.
Professor Murakami explains: “Periodontal disease is an infectious disease and a progressive chronic disease. It is not a disease that one can avoid if one works out to keep fit. The core of its prevention and treatment is to regularly keep the mouth clean and remove dental plaque. However, even if inflammation of periodontal tissue can be cured by treatment and progression of the disease stopped, periodontal tissue, such as the alveolar bone, cannot be restored once it is lost. Special treatment to turn the clock back is necessary to recover the lost periodontal tissue, known as regenerative therapy.”
Research was started in the 1990s
It was in the early 1990s when Professor Murakami began to engage in research on treatment to “turn back the clock” shortly after he returned from the National Institute of Health (NIH), USA. Conventional dental treatment was mainly removing diseased tissues and replacing them with artificial materials. Around this time, however, research aiming to activate cells at damaged sites using proteins collectively called cytokines and to restore lost functions was conducted worldwide.
Professor Murakami reflects: “Workers called stem cells that can regenerate damaged tissues are present in our bodies even after we have grown into adults. For example, if we selectively collect stem cells from cells of the periodontal ligament after extraction of a wisdom tooth, they differentiate into cells that make bone and cementum. If we culture them in a different environment, they also develop into fat cells. Thus, we learned that the periodontal ligament contains baby cells or undifferentiated mesenchymal stem cells that have the potential to become different cells in the future. However, we are not yet fully utilizing the potential of such cells. Researchers are thinking that periodontal tissue can be regenerated if these cells can be stimulated properly and are trying to realize this possibility.”
In such a trend to renovate the concept of dental treatment, Professor Murakami and his collaborators directed their attention to a cytokine called basic fibroblast growth factor (FGF-2) because it not only induces the proliferation of stem cells and cells that produce materials, including collagen, but also has the activity to potently induce angiogenesis. This decision was based on the idea that “even if cured, tissue does not regenerate unless nutrition is consistently supplied. For this, formation of new blood vessels is indispensable.”
Professor Murakami and his collaborators obtained cooperation from pharmaceutical companies interested in this research and carried out animal experiments. They administered FGF-2 to beagle dogs with periodontal disease. After a short time, when they turned over the gingiva, they immediately noticed that bone was restored there. Encouraged by this result, they patiently continued studies to evaluate the mechanism of tissue regeneration, safety of the agent as a drug, etc.
It is not “magic water”
Then, in 2001, a clinical trial as a step toward clinical application started. However, the research thereafter was filled with obstacles. There were overseas examples using GTR and Emdogain®
as cytokines to induce regeneration of periodontal tissue. However, they were all classified as “medical devices” and not “drugs”.
“There were no drugs demonstrated to be effective for tissue regeneration even in the field of medicine. Obtaining approval as a drug is far more difficult than obtaining approval as a medical device. I strongly wished for drugs for tissue regeneration to be approved, but it was highly difficult to have unprecedented cases approved. The discussion started with the question ‘To begin with, is such a drug really necessary?’ and strong concern was expressed regarding ‘strong side effects?’ How should drug effects be evaluated? How should the patient’s condition be assessed? We had to create a wide range of conventions and rules by ourselves in order for the treatment to be acknowledged according to international standards.”
By overcoming such problems one by one, we managed to bring “Regroth”, the first periodontal tissue regeneration agent, to patients through large-scale clinical trials to confirm its safety and efficacy. A quarter of century had passed since the research project was initiated.
However, this was not a goal. “Regroth” was originally a drug aimed to activate the patients’ own stem cells and was targeted to moderate periodontitis. Its effectiveness is limited if the disease is severe or if stem cells themselves are deficient due to old age.
Presently, therefore, we are investigating a method to transplant stem cells themselves.
Professor Murakami said “We are focusing our attention on stem cells derived from fat tissue. We make an incision approximately 1 cm long on the side of the patient’s navel and aspirate several tens of milliliters of fat tissue. We collect stem cells from it, proliferate them, and transplant them to sites of bone defect. We first want to establish this treatment and use it to help patients with severe periodontitis.” This method has already been applied to a few patients, reportedly with promising results.
Although periodontal tissue regeneration therapy has a great potential, Professor Murakami warns that “regeneration-inducing agents are never ‘Magic Water’” because “conventional treatments for periodontal disease are makeshift attempts to prevent the destruction of periodontal tissue, which advances with time like a landslide. Regenerative medicine turns the clock back a little bit. It never restores steel-like gingiva or alveolar bone. If we drop our guard, the condition deteriorates. Careful brushing is the basis of prevention and treatment.”
At lectures for citizens, he always asks the participants
“Why don’t you take this chance and get a new toothbrush? One at a reasonable price by a reasonable manufacturer will do. You can take one step forward for your health with an investment of \200-300.”
What is research to Professor Murakami?
The endeavor to reach the truth that no one knows. It was during my studies overseas when I was unable to obtain my desired experimental results and was depressed. As I was doing an experiment in the laboratory alone late at night, I finally got the results expected from the hypothesis. I was excited and showed the results to a Japanese colleague at the laboratory. At that time, he said “You are the only one who knows this truth.” His words still linger in my mind.
Professor of the Graduate School of Dentistry, Osaka University
Interview held in December 2019
