Development of the world's first integrated extracorporeal circuit, UTOpiA system, using hypoimmunogenic liver organoids
Significantly improved life prognosis in animal models of acute liver failure (ALF)!
- Developed the world's first integrated extracorporeal circuit, UTOpiA system, which combines iPSC-derived hepatocyte-like cell (iHLC) organoids and granulocyte and monocyte/macrophage apheresis.
- The UTOpiA system exerts multiple effects, such as reducing hepatic disfunction, compensating for liver function, and promoting liver regeneration.
- Successfully achieved a significant improvement in survival rates in models of acute-on-chronic liver failure (ACLF) and acute liver failure (ALF), which have high fatality rates.
- Development is undergoing toward clinical trials within the next few years, and it is expected that innovative regenerative medicine products will be put to practical use in the future.
Outlines
A research group including Dr. Hitomi Yamaguchi (PhD student) at the Science Tokyo Graduate School of Medical and Dental Sciences, Associate Professor (Lecturer) Yosuke Yoneyama at the Graduate School of Medicine of the University of Osaka, and Professor Takanori Takebe (Premium Research Institute for Human Metaverse Medicine of the University of Osaka/Professor at the Human Biology Research Unit of Institute of Integrated Research, Science Tokyo) has developed the UTOpiA system, an integrated extracorporeal circuit that incorporates iPSC-derived hepatocyte-like cell (iHLC) organoids.
Acute-on-chronic liver failure (ACLF) is a disease that develops in patients with chronic liver failure such as cirrhosis due to trigger including infection, gastrointestinal bleeding, or excessive alcohol consumption, and causes a rapid decline in liver function with 28-day mortality rates. That’s why establishing an effective treatment other than organ transplantation has been a major challenge.
In this study, the research group developed a whole blood extracorporeal circulation system called UTOpiA that combines granulocyte and monocyte/macrophage apheresis (GMA) with HLA gene-modified iPSC-derived hepatocyte-like cell (iHLC) organoids. The therapeutic effects of UTOpiA were examined in rat models of ACLF and acute liver failure (ALF). The results showed that it reduced coma, improved hyperammonemia and hyperbilirubinemia, and suppressed systemic inflammation, significantly improving survival rates. Furthermore, it was confirmed that the treatment promoted a regenerative response in the livers of the animals.
These results suggest that UTOpiA may be a new therapeutic option for severe liver failure by simultaneously providing anti-inflammatory effect, metabolic and synthetic functions, and regeneration-promoting effects. The research group plans to begin clinical trials within the next few years, and it is expected that this will lead to the development of innovative regenerative medicine products that will help patients with severe liver failure in the future.
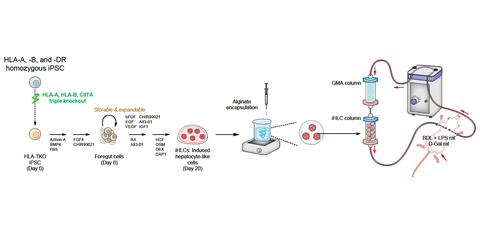
Fig. 1 Overview of the UTOpiA system and its therapeutic effects
A: Components and conceptual diagram of UTOpiA
B: Therapeutic effect on ACLF
Credit: Takanori Takebe
Research Background
Acute-on-chronic liver failure (ACLF) is a dangerous disease that occurs when a person with chronic liver disease such as cirrhosis suddenly deteriorates, causing multiple organ dysfunction due to some trigger such as infection, gastrointestinal bleeding, or excessive alcohol consumption, and liver function deteriorates rapidly within 28 days. In severe cases, the survival rate is low at around 20%, making it difficult to establish effective treatment methods. In particular, although research into intensive care is progressing, there is currently no established method to fundamentally treat the serious systemic inflammatory response syndrome and liver dysfunction that occur with this clinical condition.
Currently, liver transplantation is the only radical treatment, but there is a shortage of donor organs, and many patients die while waiting for a transplant. Previously, several attempts have been made to treat the disease by processing blood outside the body to suppress inflammation or by artificially supplementing liver function, but it has been difficult to suppress inflammation, and no treatment has been able to simultaneously fully supplement the liver's metabolism.
Research Contents
In this study, the research group developed an integrated extracorporeal circuit, UTOpiA system, which combines granulocyte and monocyte/macrophage apheresis (GMA) with newly created iPSC-derived hepatocyte-like cell (iHLC) organoids. This system consists of two columns connected in series: a GMA column, which removes white blood cells that cause inflammation, and a column filled with genome-edited alginate-encapsulated iHLCs to make them less likely to cause rejection (Fig. 2).
Fig. 2 Overview of iHLC creation method and verification image using UTOpiA extracorporeal circulation
Credit: Takanori Takebe
The research group first created iHLCs from HLA-A, HLA-B, and CIITA triple knockout iPSCs which involved in rejection. iHLCs retain the main liver functions, such as albumin production, bilirubin uptake, and urea cycle function, and have been confirmed to have low expression of immune-stimulating HLA molecules. Next, the researchers devised a method to safely bring iHLC into contact with blood by alginate-encapsulation into a small gel-shaped cupsule, a method used in making artificial salmon roe. By connecting an iHLC column filled with this gel and a GMA column in series, an extracorporeal circulation system that allows direct blood return was created, and they named it UTOpiA.
The therapeutic effect of UTOpiA has been confirmed in two animal models. First, they induced acute liver cirrhosis in rats by intraperitoneal administration of lipopolysaccharide (LPS) in a bile duct ligation (BDL) model and then examined the effects of this model on a state similar to severe human liver failure (ACLF model). As a result, the survival rate in the untreated group dropped to less than 10% within 48 hours, whereas the highest survival was observed in the UTOpiA-treated group (88.9%) (Fig. 1). Furthermore, it was shown to improve indicators of kidney damage (creatinine levels) and reduce symptoms such as coma, liver function, hyperammonemia, hyperbilirubinemia, and systemic inflammation. After UTOpiA treatment, the increase in blood indicators indicating liver damage (AST, ALT, ammonia, etc.) was suppressed, and liver tissue damage was also reduced. Similar effects were observed in another rat model of D-galactosamine-induced ALF.
Interestingly, UTOpiA treatment has been shown to restore metabolic and energy production functions in liver cells in animal models with liver failure. For example, the results of comprehensive gene expression analysis showed that genes involved in the metabolism of amino acids and fatty acids were mainly activated. Furthermore, the concentration of hepatocyte growth factor (HGF) in the blood increased and the area around the necrotic cells recovered, demonstrating that UTOpiA also has the effect of promoting the proliferation of hepatocytes in livers with ACLF and helping to regenerate damaged tissue (Fig. 3).
Fig. 3 Effects by UTOpiA treatment promoting the regeneration of recipient hepatocytes
Credit: Takanori Takebe
Social Impact of the Research
The results of this study are expected to make the integrated extracorporeal circuit UTOpiA system an innovative treatment for severe liver failure, including ACLF, which has a high mortality rate. Currently, the research group is working to establish mass production methods and verify the system in large animal tests in preparation for commercialization, with the aim of starting clinical trials within the next few years.
Notes
The article, “Reversal of ACLF and ALF by whole blood extracorporeal system with HLA-depleted liver organoids and granulocyte-monocyte apheresis,” was published inJournal of Hepatology (online) at DOI: https://doi.org/10.1016/j.jhep.2025.08.038

