Existence of dermatomyositis sine dermatitis and its association with anti-NXP-2 autoantibodies verified
A group of researchers from the National Center of Neurology and Psychiatry (NCNP), the University of Tsukuba and Osaka University has demonstrated that dermatomyositis (DM) sine dermatitis (DMSD) does exist and is significantly associated with anti–nuclear matrix protein 2 (anti-NXP-2) autoantibodies.
Autoantibodies, proteins produced by the immune system, recognize a person’s own proteins and attack them as if they were invaders. In the case of myositis, autoantibodies are directed against skeletal muscle, so myositis is called an autoimmune disease.
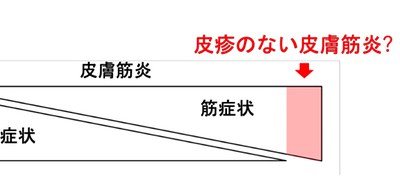
Dermatomyositis (DM), an inflammatory myopathy, causes muscle weakness and a skin rash and can be divided in two groups: clinically amyopathic DM (CADM) and DM without dermatitis, or dermatomyositis sine dermatitis (DMSD).
Idiopathic inflammatory myopathy (IIM) are a group of chronic, autoimmune conditions affecting primarily the proximal muscles. Conventionally, IIM was roughly classified into two specific kinds: polymyositis (PM) that causes muscle weakness and dermatomyositis (DM) that causes muscle weakness plus a skin rash; however, more appropriate categorization has been taken in recent years.
There are 5 myositis-specific autoantibodies (MSA) for DM and there is usually a close association between particular autoantibodies and a set of clinical symptoms. For example, CADM is associated with anti–melanoma differentiation-associated gene 5 (MDA5) antibodies. However, since DMSD was categorized as PM, reports on DMSD are scarce and the concept of the disease has not been widely accepted.
In this study, the researchers confirmed the existence of DMSD using a sensitive and specific pathological marker of DM, myxovirus resistance protein A (MxA). In a cohort study of 182 patients with DM who were positive for DM-specific autoantibodies, 14 (8%) had DMSD. Since the 14 patients didn’t have a skin rash at the time of muscle biopsy, they were diagnosed with DMSD.
While 28% of DM patients (47 of 168) with a skin rash were positive for anti-NXP-2 autoantibodies, among the 14 patients with DMSD, 12 (86%) were positive for anti-NXP-2 autoantibodies. This indicated a significant association between anti-NXP-2 autoantibodies and DMSD.
The researchers further assessed the follow-up data of 14 patients with DMSD. Using diagnosis criteria for CADM, they diagnosed DMSD based on the absence of a skin rash at the time of muscle biopsy. A diagnosis of CADM was made in case the amyopathic period lasted for 2 years or more. Even if they excluded patients with DMSD with an adermopathic period of less than 2 years, they couldn’t discount the evidence that unadjusted logistic regression analyses (LRA) revealed a statistically significant association between anti-NXP-2 autoantibodies and DMSD in 9 patients with DMSD.
Since therapy effective against DM’s primary pathogenic mechanism has recently been developed, the importance of diagnosing DM by distinguishing DM from PM and other forms of myositis has increased. This group’s achievements will enable to make a correct diagnosis of DM, which will improve treatment for patients who were previously diagnosed with PM.
Figure 1
The article, “Association of Dermatomyositis Sine Dermatitis With Anti-Nuclear Matrix Protein 2 Autoantibodies,” was published in JAMA Neurology at DOI: https://jamanetwork.com/journals/jamaneurology/article-abstract/2764337.
Related Links
Dermatology, Department of Integrated Medicine, Graduate School of Medicine, Osaka University (link in Japanese)
