Pathological regression of lymph nodes better predicts esophageal cancer survival
A group of researchers led by Osaka University established a new pathological grading system to evaluate the therapeutic effect of neoadjuvant chemotherapy (NAC) for metastatic lymph nodes (LNs) removed in esophageal cancer (EC) surgery, demonstrating that the system predicts recurrence and prognosis in EC patients better than conventional systems. Their research results were published in Annals of Surgery .
The majority of patients with progressive EC have LN metastases. Such patients usually receive NAC before surgery. Since patients who showed good response to NAC are known to have a favorable prognosis, it is important to accurately evaluate the therapeutic effect of NAC.
Routine pathological evaluation of NAC is conducted for the therapeutic effect on the primary tumor (PT). PT regression grade is determined by calculating the proportion of viable tumor area within the whole tumor bed area. Evaluations are classified into four categories according to the proportion. A high grade shows a high therapeutic effect of NAC. This tumor regression grade classification is a good indicator for predicting recurrence and prognosis.
Because metastatic status of LN, which is known to be associated with systemic micrometastases, serves as a more reliable indicator of patient survival compared with PT progression in EC patients, this group hypothesized that, in patients who have undergone NAC for EC, the pathological LN response might be a better prognostic factor than the pathological PT response.
Among 371 eligible patients, 52 had negative LNs with no evidence of regression. The researchers evaluated the therapeutic effect of NAC for the remaining 319 patients by grading pathological tumor regression into four categories according to residual tumor per tumor bed.
For all metastatic LNs, the researchers generated a total LN regression grade according to the proportion of the summed viable tumor area relative to the summed tumor bed area (Figure 1I). 153 patients (48.0%) exhibited better response and 191 (59.9%) showed a difference in response between the PT and LN regression grades. Specifically:
• Prognosis varied depending on the total LN regression grade (Figure 2A) and the recurrence-free survival (RFS) rate among responders was significantly better than that of non-responders.
• Although the therapeutic effect was significantly correlated with survival in both PT (Figure 2B) and LN (Figure 2C), the survival difference was more prominent in LN than PT.
• LN regression grade was an independent prognostic factor of the duration of survival.
• The rates of hematogenous recurrences and lymphatic recurrences were significantly lower in responder compared with non-responder in both PT and LN. However, these differences were more remarkable in LN response.
These findings show that pathological assessment of all metastatic LNs is excellent in predicting prognosis and disease recurrence in patients who undergo NAC for EC.
Lead author Professor Tomoki Makino says, “We’ve found that it is possible to predict disease recurrence and prognosis by performing pathological assessment of all metastatic LNs. Moving forward, this will enable ‘tailor-made’ treatment according to the pathological assessment of all metastatic LNs, eventually improving treatment performance of EC.”

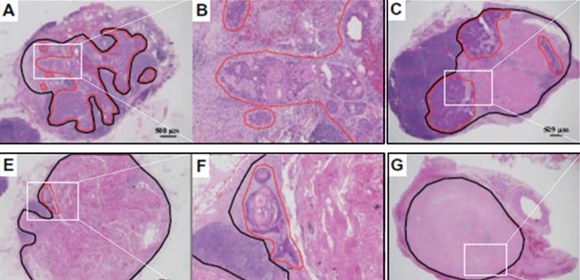
Figure 1. Assessment of tumor regression according to LN regression grading (lymph nodes (LNs) stained with hematoxylin and eosin)
(A, B) Grade I: Viable tumor cells are observed in over 50% of the tumor bed area. (C, D) Grade II: Viable tumor cells are observed in 10%–50% of the tumor bed area. (E, F) Grade III: Viable tumor cells are observed in <10% of the tumor bed area. (G, H) Grade IV: No viable tumor cells observed in the tumor bed area. (I) Schematic representation of a formula used for calculating the total LN regression grade.
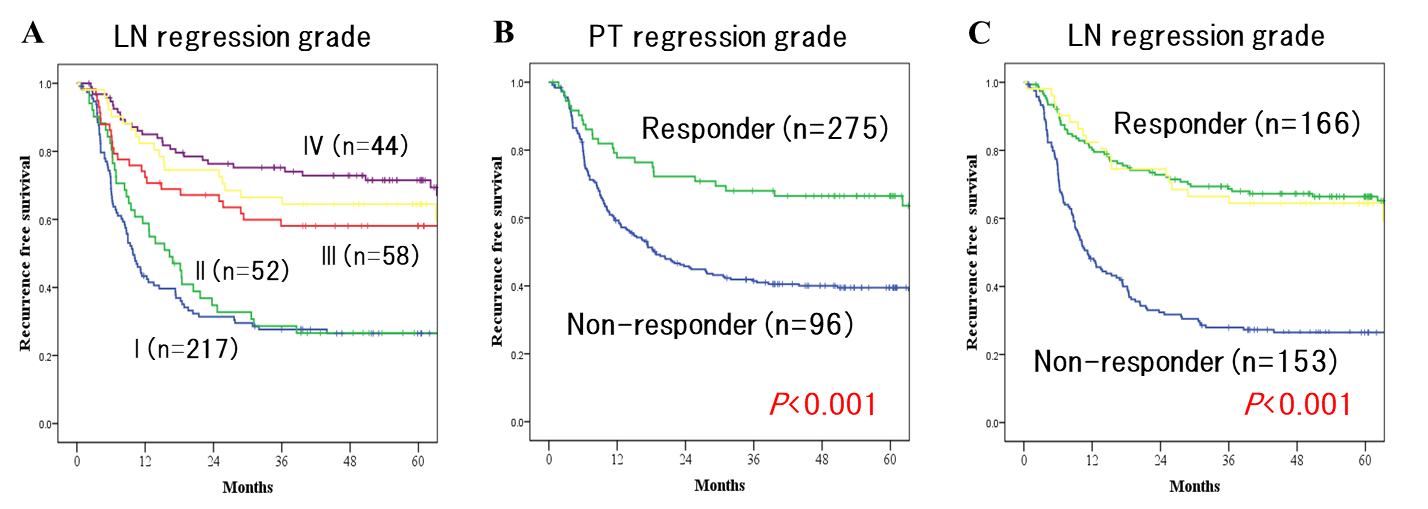
Figure 2. Kaplan-Meier recurrence-free survival (RFS) according to (A) LN regression grade, (B) non-responders and responders in terms of primary tumor (PT) regression grade, and (C) non-responders and responders in terms of LN regression grade. The yellow curves represent patients who showed no evidence of regression or previous tumor involvement. The grade of pathological LN response gradually stratifies patient survival and is a better predictor of long-term survival than that of PT response.
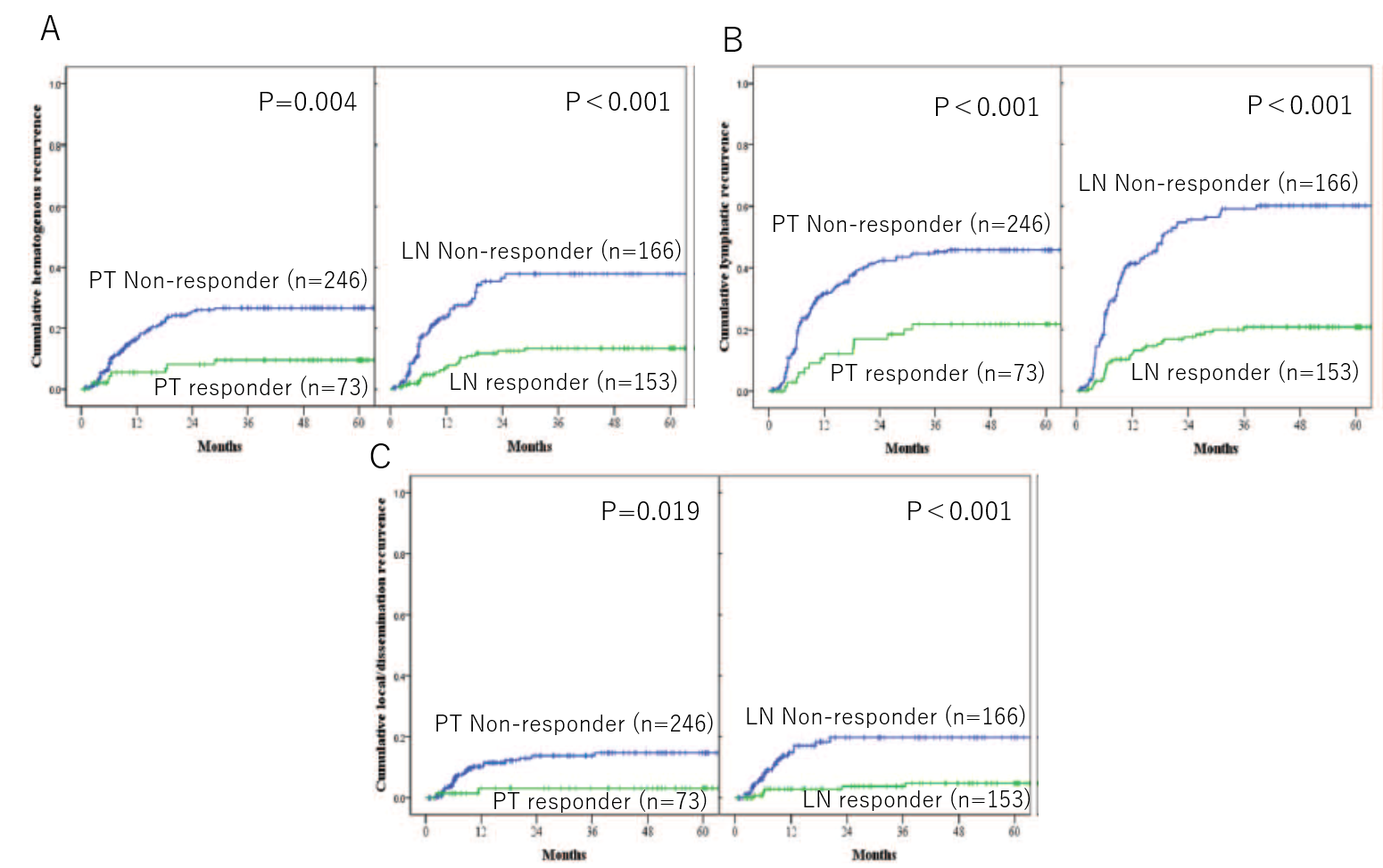
Figure 3. Kaplan-Meier cumulative recurrences in 319 patients with clinically positive LNs according to PT regression grade and total LN regression grade: (A) hematogenous recurrence, (B) lymphatic recurrence, and (C) local or dissemination recurrence.
In terms of total LN regression grade, compared to non-responders, responders exhibit significantly lower rates of hematogenous, lymphatic, and local or dissemination recurrences, and these differences are more prominent than responders in terms of PT regression grade.
The article, “Pathological regression of lymph nodes better predicts long-term survival in esophageal cancer patients undergoing neoadjuvant chemotherapy followed by surgery,” was published in Annals of Surgery at DOI: https://doi.org/10.1097/SLA.0000000000004238 .
Related Links
