Interleukin-1α causes people to choke on air
Researchers have pinpointed specific molecular events that could explain allergic reactions to air pollution
Photos of cities darkened by pollution are becoming evermore common. These same cities are seeing a rise in cases of asthma and other respiratory ailments, marking a relationship between pollution and health costs. Nanoscopic particulates polluting the air enter the lungs to cause the allergic reactions. Which immune-related events in the lung lead to this response, however, are unclear.
"We found that particulates kill macrophages, which then go on to release interleukin-1 α (IL-1 α )", explains Etsushi Kuroda, who first-authored a new study in Immunity that indicates IL-1 α triggers a series of events that causes respiratory illnesses. The release of IL-1 α in mice primed the lungs for inflammation when the mice were later exposed to an allergen. Kuroda added, "Particulates that did not kill macrophages did not cause an allergic reaction."
However, the vulnerability of macrophages to particulates remains unclear, which is why understanding the events following IL-1 α secretion may be key to prevention and treatment.
"IL-1 α secretion was followed by the formation of iBALTs. iBALTs are frequently found in infected or inflamed lungs and in patients with asthma," said Osaka University Professor Ken J. Ishii, who led the study. The increase in iBALTs led to an increase in IgE antibodies, which intensified the immune response. On the other hand, mutant mice that were insensitive to IL-1 α did not produce iBALTs and reduced IgE responses.
The presence of iBALTs would suggest that a human population could remain susceptible to high levels of asthma attacks even on clear days, as the iBALTs could form on days of high pollution, but the patient could then be exposed to the allergen much later.
This finding suggested that iBALTs could prime the lungs to an allergic reaction, which is why Ishii believes that iBALTs could make a promising therapeutic target to combat the rise of respiratory illnesses associated with air pollution. But first, he said, "we must identify the molecular signals and key chemicals that form these iBALTs."
Abstract
Particulate pollution is thought to function as an adjuvant that can induce allergic responses. However, the exact cell types and immunological factors that initiate the lung-specific immune responses are unclear.We found that upon intratracheal instillation, particulates such as aluminum salts and silica killed alveolar macrophages (AMs), which then released interleukin-1a (IL-1a) and caused inducible bronchus-associated lymphoid tissue (iBALT) formation in the lung. IL-1a release continued for up to 2 weeks after particulate exposure, and type-2 allergic immune responses were induced by the inhalation of antigen during IL-1a release and iBALT formation, even long after particulate instillation. Recombinant IL-1a was sufficient to induce iBALTs, which coincided with subsequent immunoglobulin E responses, and IL-1-receptor-deficient mice failed to induce iBALT formation. Therefore, the AM-IL-1a-iBALT axis might be a therapeutic target for particulateinduced allergic inflammation.
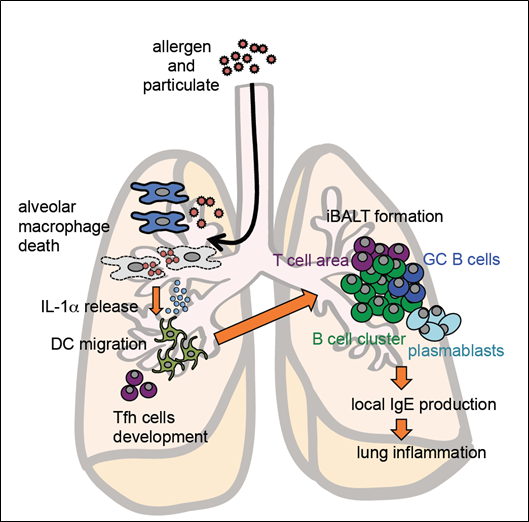
Model of particulate-induced allergic inflammation in the lungs
To learn more about this research, please view the full research report entitled “ Inhaled Fine Particles Induce Alveolar Macrophages Death and Interleukin 1a Release to Promote Inducible Bronchus-Associated Lymphoid Tissue Formation ” at this page of the Immunity website.
Related links
